News

Pelvic Floor Muscle Training: Why Clinics Are Investing in Advanced Pelvic Health Devices
Pelvic floor muscle training is rapidly becoming a core service in modern clinics as demand for non-invasive pelvic health solutions continues to rise. Conditions such as urinary incontinence, postpartum muscle weakness, and age-related pelvic floor decline now affect a broader patient population than ever before, driving clinics to seek more effective and reliable treatment options.
While traditional pelvic floor exercises offer limited and inconsistent results, advanced pelvic health devices are transforming how clinics deliver pelvic floor muscle therapy. By providing deeper muscle activation, improved treatment consistency, and measurable outcomes, device-based pelvic floor training allows clinics to enhance patient satisfaction while unlocking new revenue opportunities in the growing pelvic health market.
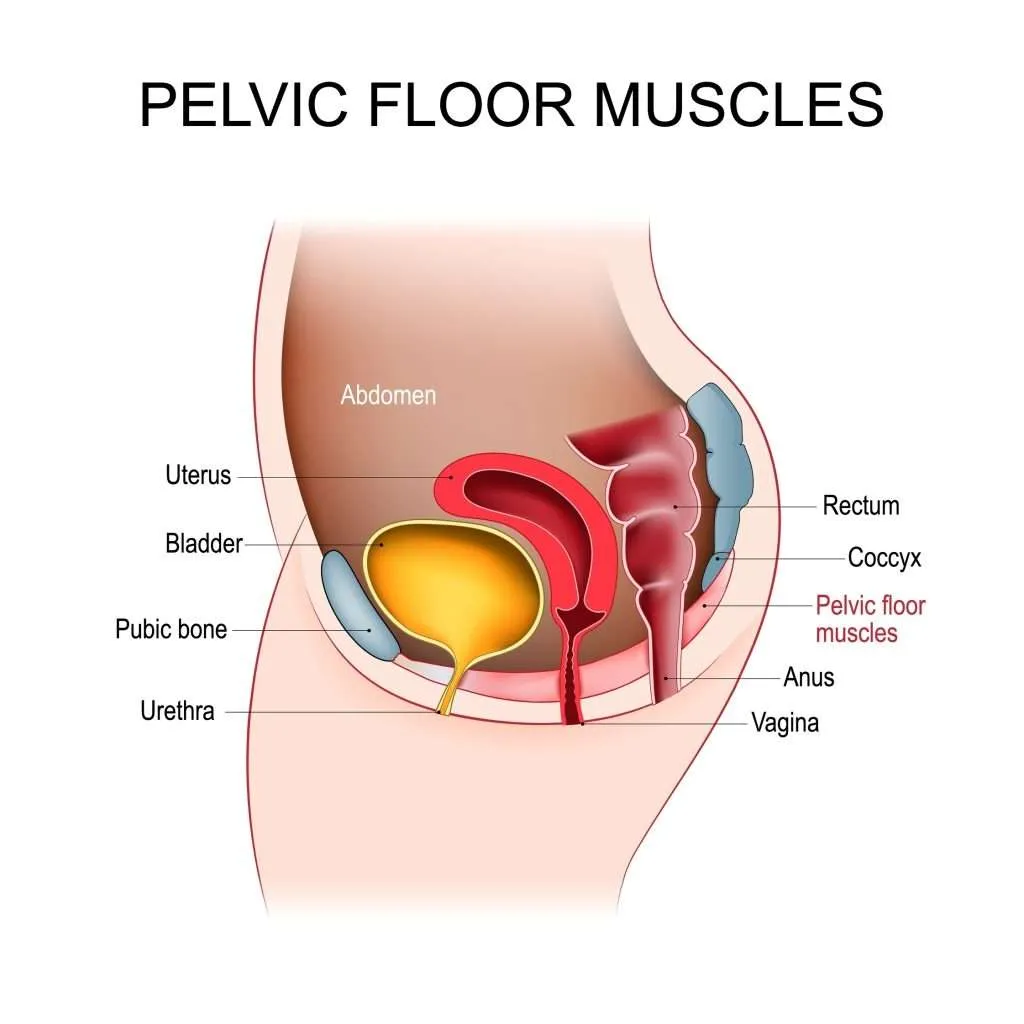
Understanding Pelvic Floor Muscles and Their Clinical Importance
What Are Pelvic Floor Muscles and Why They Matter in Pelvic Health
Pelvic floor muscles are a complex group of muscles and connective tissues located at the base of the pelvis. They form a supportive structure that stabilizes the bladder, uterus or prostate, and rectum while maintaining continence and contributing to core stability. From a clinical perspective, effective pelvic floor muscle function depends on strength, endurance, coordination, and neuromuscular control.
These muscles work continuously to support pelvic organs and respond dynamically to increases in intra-abdominal pressure during activities such as coughing, lifting, and physical movement. When pelvic floor muscles weaken or lose functional coordination, a range of pelvic health disorders may develop.
The Role of Pelvic Floor Muscles in Pelvic Health
Pelvic floor muscles play a critical role in maintaining normal pelvic function across different life stages. Clinically, pelvic floor muscle integrity is essential for:
Urinary and fecal continence
Pelvic organ support and stability
Sexual function and sensation
Postural control and core muscle coordination
Pelvic floor muscle dysfunction can affect both women and men and is not limited to postpartum or elderly populations. Factors such as pregnancy, childbirth, aging, hormonal changes, obesity, and previous pelvic surgery may all contribute to progressive muscle weakening or impaired neuromuscular activation.
Common Clinical Conditions Associated with Pelvic Floor Muscle Dysfunction
Pelvic floor muscle dysfunction is increasingly recognized as an underlying factor in several common clinical conditions, including:
Stress and urge urinary incontinence
Postpartum pelvic floor weakness
Pelvic organ prolapse (mild to moderate)
Reduced pelvic stability and functional support
Decreased quality of life related to pelvic health symptoms
As awareness of these conditions grows, pelvic floor muscle training has become an essential therapeutic strategy within pelvic health, rehabilitation, and women’s health clinics.
Why Pelvic Floor Muscle Assessment and Training Matter in Clinical Practice
Accurate assessment and targeted pelvic floor muscle training are essential for developing effective treatment plans. From a clinical standpoint, identifying muscle strength, endurance, and activation patterns allows practitioners to tailor interventions that address individual patient needs.
With increasing patient demand for non-invasive and clinically guided solutions, pelvic floor muscle training has evolved beyond basic exercise instruction. Clinics are now focusing on structured, outcome-oriented pelvic health programs that emphasize consistency, measurable improvement, and long-term functional recovery.
Limitations of Traditional Pelvic Floor Muscle Training
Challenges in Postpartum and Perinatal Care
From an obstetrics and gynecology perspective, pelvic floor muscle training is commonly recommended during pregnancy and after childbirth to support pelvic recovery. However, postpartum patients often experience fatigue, discomfort, hormonal fluctuations, and reduced neuromuscular awareness, which can limit their ability to perform pelvic floor exercises correctly and consistently.
In clinical practice, improper activation of pelvic floor muscles—such as overrecruitment of accessory muscles or insufficient deep muscle engagement—may reduce the effectiveness of traditional training approaches, particularly in early postpartum rehabilitation.
Variability in Muscle Activation and Treatment Outcomes
Pelvic floor muscle contraction is a complex neuromuscular process that is not easily mastered without guidance or feedback. In gynecological settings, clinicians frequently encounter patients who struggle to accurately identify and engage the correct muscle groups, leading to significant variability in training outcomes.
This variability can make it difficult to standardize pelvic floor muscle training protocols or to objectively evaluate treatment progress, especially when relying solely on verbal instruction or home-based exercise programs.
Limited Monitoring and Objective Assessment
Traditional pelvic floor muscle training often lacks objective assessment tools that allow clinicians to measure muscle strength, endurance, or activation patterns over time. From a gynecological care standpoint, this limitation reduces the ability to track functional improvement or adjust treatment plans based on measurable data.
Without consistent monitoring, treatment outcomes may depend heavily on patient self-reporting, which can introduce subjectivity and reduce clinical reliability in pelvic floor rehabilitation programs.
Barriers to Long-Term Adherence
Sustained pelvic floor muscle training is essential for long-term functional improvement, particularly in postpartum and aging populations. However, adherence to traditional exercise-based programs often declines over time due to lack of supervision, delayed symptom improvement, or limited patient motivation.
In gynecology clinics, these barriers highlight the need for more structured and clinically guided pelvic floor muscle training solutions that can support patient engagement while maintaining treatment consistency.
The Rise of Advanced Pelvic Health Devices
Evolving Clinical Demand for Non-Invasive Pelvic Floor Solutions
As awareness of pelvic floor dysfunction continues to grow, clinics are facing increasing demand for non-invasive pelvic floor treatments that deliver reliable and reproducible results. In gynecology, women’s health, and rehabilitation settings, pelvic floor muscle training is no longer viewed solely as an adjunct therapy but as a primary intervention for functional pelvic health management.
This shift has accelerated the adoption of advanced pelvic health devices designed to support structured pelvic floor muscle therapy under clinical supervision, addressing the need for consistency, safety, and efficiency in patient care.
How Advanced Pelvic Health Devices Support Pelvic Floor Muscle Training
Modern pelvic health devices utilize controlled energy-based or neuromuscular stimulation technologies to activate pelvic floor muscles in a precise and targeted manner. By inducing standardized muscle contractions, these systems support effective pelvic floor muscle engagement that may be difficult to achieve through voluntary training alone.
From a clinical perspective, device-assisted pelvic floor muscle training enables practitioners to deliver uniform treatment protocols while maintaining adjustable parameters tailored to individual patient needs and tolerance levels.
Improved Treatment Standardization and Clinical Efficiency
One of the key advantages of advanced pelvic health devices is their ability to standardize pelvic floor muscle therapy across different patient populations. In busy clinical environments, standardized treatment protocols reduce variability in care delivery and help ensure consistent therapeutic quality.
Additionally, device-based pelvic floor muscle training can be integrated into routine clinical workflows with minimal disruption, allowing clinics to optimize appointment scheduling while maintaining a high level of clinical oversight.
Expanding the Scope of Pelvic Health Services in Clinics
The integration of advanced pelvic health devices has enabled clinics to broaden their pelvic floor treatment offerings beyond traditional exercise-based programs. These technologies support comprehensive pelvic health services, including postpartum recovery programs, preventive pelvic floor care, and long-term muscle maintenance strategies.
As a result, pelvic health devices are increasingly viewed as strategic clinical investments, supporting both improved patient outcomes and sustainable growth in pelvic health services.
Clinical Benefits of Device-Based Pelvic Floor Muscle Training
Enhanced Muscle Activation and Functional Engagement
Device-based pelvic floor muscle training enables controlled and consistent activation of deep pelvic floor muscles that may be difficult for patients to engage voluntarily. Through standardized stimulation patterns, these treatments support effective muscle contraction and relaxation cycles, contributing to improved strength, endurance, and neuromuscular coordination.
From a clinical standpoint, enhanced muscle activation plays a critical role in restoring functional pelvic support and improving continence-related outcomes.
Improved Consistency and Reproducibility of Treatment
One of the key clinical advantages of device-assisted pelvic floor muscle training is the ability to deliver reproducible treatment sessions. Unlike exercise-only programs, device-based therapy follows defined parameters that reduce variability between sessions and across different patient populations.
This consistency allows clinicians to implement structured treatment plans and evaluate progress with greater confidence, supporting higher standards of clinical care.
Objective Monitoring and Treatment Precision
Advanced pelvic health devices offer measurable treatment parameters that support objective clinical assessment. Adjustable intensity levels and session timing allow practitioners to tailor pelvic floor muscle training based on individual patient tolerance and therapeutic goals.
Objective monitoring supports data-informed decision-making, enabling clinicians to optimize treatment protocols and adjust therapy as pelvic floor muscle function improves.
Broader Patient Suitability and Clinical Accessibility
Device-based pelvic floor muscle training is suitable for a wide range of patients, including postpartum individuals, aging populations, and patients with limited ability to perform voluntary pelvic floor exercises. The non-invasive nature of these treatments allows clinics to offer pelvic floor muscle therapy with minimal discomfort and downtime.
This broader clinical accessibility supports inclusive pelvic health care and expands treatment options for patients at different stages of pelvic floor dysfunction.
Support for Long-Term Functional Improvement
Consistent and structured pelvic floor muscle training is essential for maintaining long-term pelvic function. Device-assisted therapy supports ongoing muscle conditioning and functional maintenance, helping reduce symptom recurrence and supporting sustained clinical outcomes.
By integrating device-based pelvic floor muscle training into comprehensive pelvic health programs, clinics can deliver more reliable and durable therapeutic results.
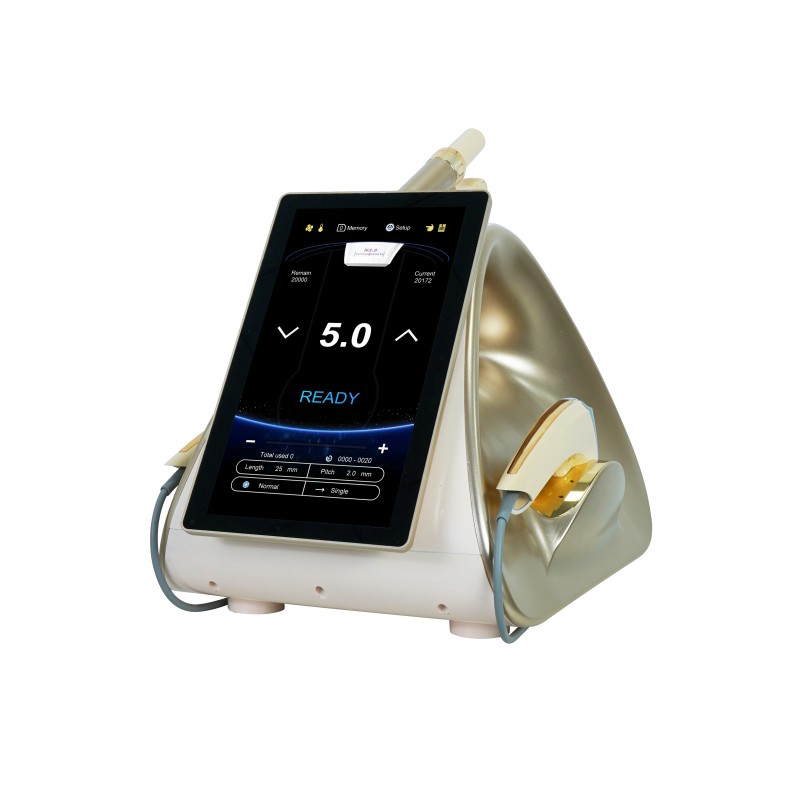
Recommended Pelvic Health Device for Clinics
To help clinicians deliver advanced pelvic floor muscle training with reliable results, the PelviTone EMS Chair by Krysmed stands out as a modern, evidence‑aligned solution for pelvic health practice.
Optimal Health Electromagnetic Chair – PelviTone EMS Chair
The PelviTone EMS Chair is a non‑invasive pelvic floor rehabilitation system designed for clinical use in women’s health, gynecology, urology, and rehabilitation clinics. It uses advanced HIFEM (High‑Intensity Focused Electromagnetic) technology, delivering electromagnetic stimulation deep into the pelvic floor muscles to achieve intense, controlled contractions—equivalent to thousands of Kegel exercises in a single session.

PelviTone EMS Chair – Key Clinical Advantages for Clinics
| Category | Clinical Benefits |
|---|---|
| Deep Muscle Activation | HIFEM technology penetrates deep pelvic floor layers that traditional exercise can’t reliably reach, supporting stronger functional improvements. |
| Non-Invasive & Painless | Treatment is fully clothed, requires no recovery time, and is suitable for a broad range of patients (postpartum, aging populations, urinary incontinence, etc.). |
| Efficient Treatment Sessions | Typical sessions are around 30 minutes, enabling high patient throughput without compromising quality of care. |
| Clinically Meaningful Results | Facilitates repeated supramaximal muscle contractions, supporting improved bladder control, enhanced pelvic support, and restored intimate health. |
| Ideal for Clinics | Designed for clinics to expand pelvic health services, offer premium technology-driven therapy, and improve patient satisfaction with measurable outcomes. |
This device integrates smoothly into women’s health and rehabilitation programs, helping clinics differentiate their service offerings and support better functional outcomes for patients.
Conclusion
Investing in advanced pelvic health devices allows clinics to provide effective, non-invasive pelvic floor muscle training with measurable outcomes. By integrating the PelviTone EMS Chair into clinical practice, clinics can enhance patient satisfaction, expand pelvic health services, and achieve consistent, functional improvements in pelvic floor strength.
Contact Krysmed today to elevate your clinic’s pelvic health offerings—learn more about the PelviTone EMS Chair and start delivering premium, technology-driven pelvic floor therapy to your patients.
Our Contact
Ready to Elevate Your Business with Krysmed?
Let’s discuss your needs and find the best solution for your business. Our experts are here to provide personalized recommendations tailored to your business needs.
-
Call For Inquiry
-
Send Us Email
info@krysmed.com
Get A Custom Quote Now!
We value your privacy and guarantee a prompt, professional reply.